Pearl #1: Select Your Patient Correctly
We feel this is the most critical part of the pathway. A poorly screened patient may suffer from irreparable harm, resulting in lifelong side-effects.
Be very cautious and possibly avoid operating on:
- Patients with generalized hyperhidrosis
- Patients with a HSS of 1 or 2
- Patients with scalp hyperhidrosis
- Patients with hyperthyroidism
- Patients with inadequately treated anxiety
- Patients who wake up complaining of the bed being soaked
- Patients with morbid obesity
Step 1: Patient and Surgeon Positioning and Port Placement
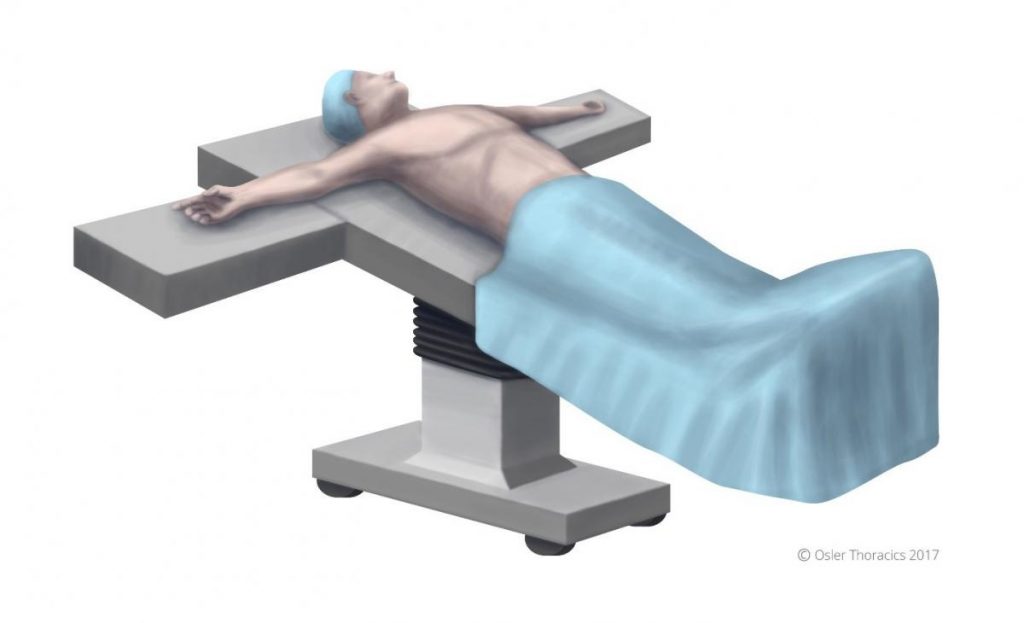
Figure 1: Patient positioning.
The patient is positioned supine, in steep reverse Trendelenburg. This will optimize exposure of the superior sulcus. The arms are abducted slightly less than 90°, and a footboard is placed to prevent the patient from sliding off the bed.
Airway management: For patients with axillary hyperhidrosis we typically place a double lumen endotracheal tube to improve exposure of the T5 ganglion. Otherwise, we use a standard single lumen ETT with insufflation.
Port Placement

Figure 2: Port placement.
Two 5 mm ports are placed:
- Infra-mammary port, anterior axillary line. The location can be modified slightly and placed in a skin-crease. Once this port is placed, the pleural space is insufflated to 8mmhg
- Within the lower part of the axilla, mid axillary line. This will function as your working port.
Pearl #2: Location of Sympathetic Interruption
| Location of Hyperhidrosis | Level of Sympathetic Interruption (R=rib level) |
|---|---|
| Palmar | R3 & R4 |
| Axillary | R4 & R5 |
| Palmar and Axillary | R3 & R4 |
| Facial Flushing | T2 |
Pearl #3: Count Ribs Correctly
Always palpate the first rib.

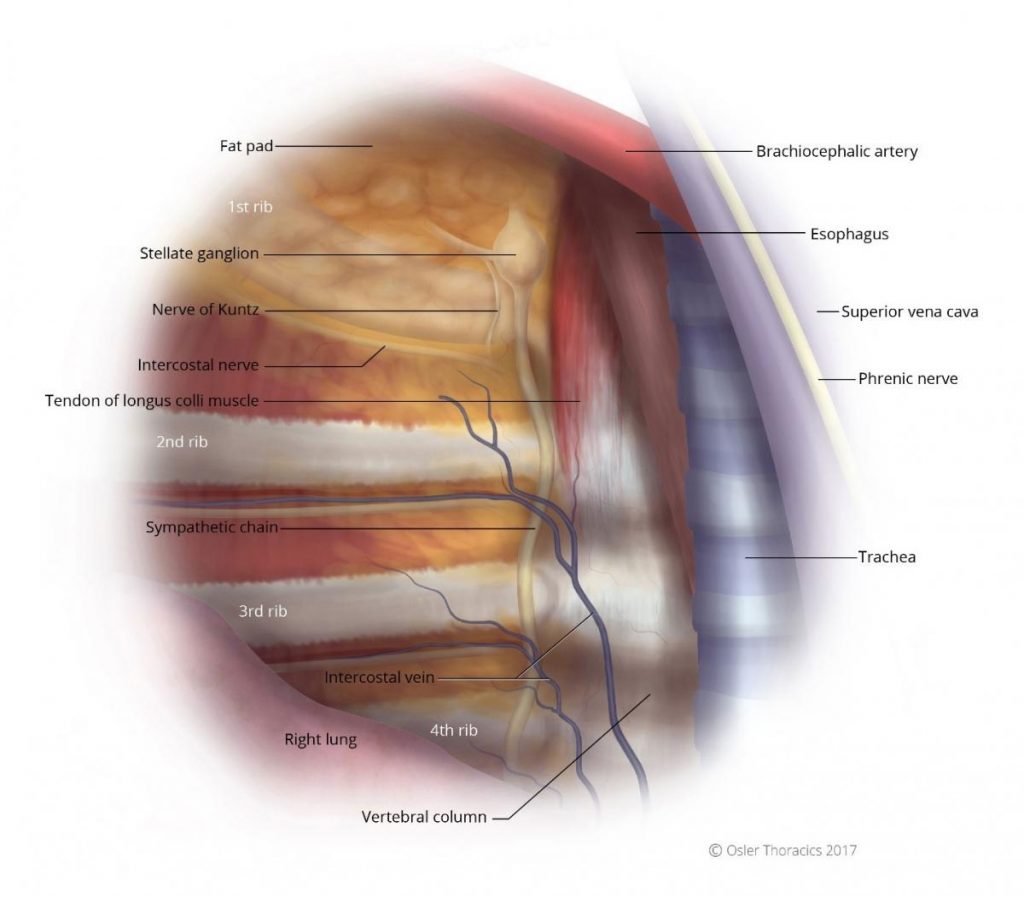
Figure 3: Right intrathoracic view, notice the first rib is often obscured by a fat pad. 
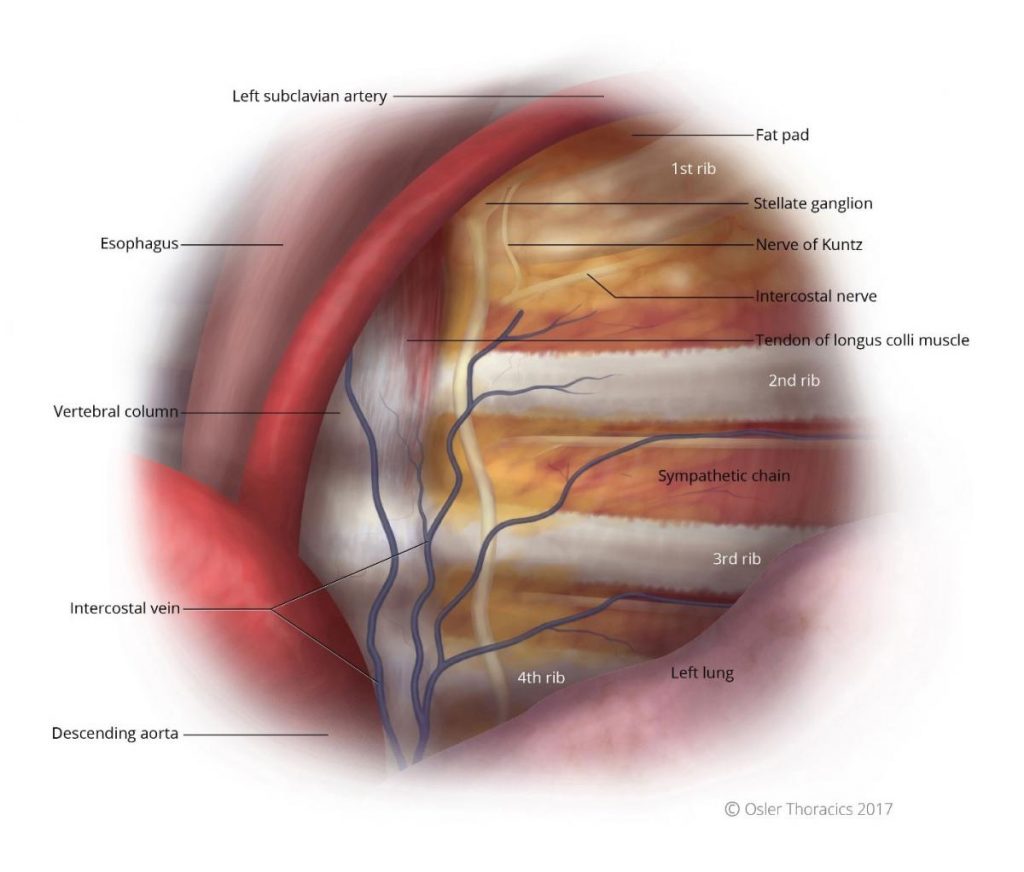
Figure 4: Left intrathoracic view, notice the first rib is often obscured by a fat pad.
Pearl #4: Beware Fascia Overlying the Longus Colli Muscle
The sympathetic chain is a white cord that runs parallel to the vertebral body, underneath the parietal pleura, and anterior to the costo-vertebral joint (see figures 3 and 4). Slightly more medial to the chain is a tendon with similar thickness and colour as that of the sympathetic nerve. This has been shown by Singh et al. to be responsible for surgical failures.
Pearl #5: Ablate the Nerve of Kuntz
The Nerve of Kuntz is an ascending rami between the second and first intercostal nerve that provides an alternative pathway for post-ganglionic fibers to reach the brachial plexus. It is surprisingly common, located 1-2 cm parallel to the sympathetic chain and the R2 and R1 level (see figures 3 and 4). Failure to identify and cauterize this aberrant nerve may lead to surgical failure.
The Azygous Lobe:
A successful ETS requires a clear view of the superior mediastinum and of the sympathetic nerve and ganglia in relation to the costal heads posteriorly, the subclavian artery superiorly, and (on the right side) the superior vena cava medially and the azygous vein inferiorly. The presence of a congenital mesoazygous web—which suspends the azygous vein and splits off an azygous lobe of the lung—can completely obscure the view of the superior sulcus that is necessary for a successful sympathectomy procedure.
The web can obscure the sympathetic nerve especially around T3. In most cases the nerve can be seen laterally to the takeoff of the web, however in some cases the nerve may be completely obscured. In these cases reflection of the web with control of the suspended azygous vein may be necessary.